Hysterectomy
What is a hysterectomy?
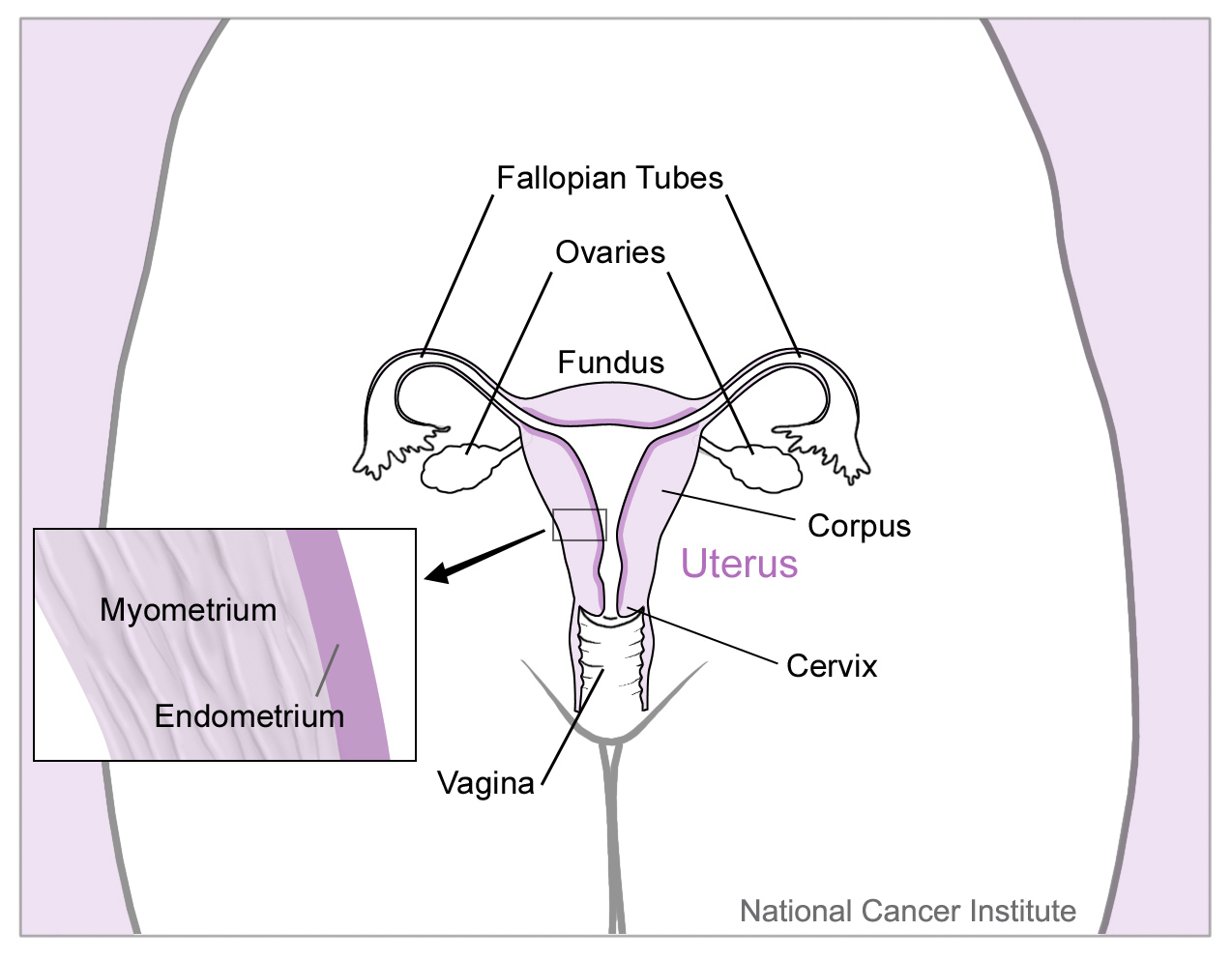
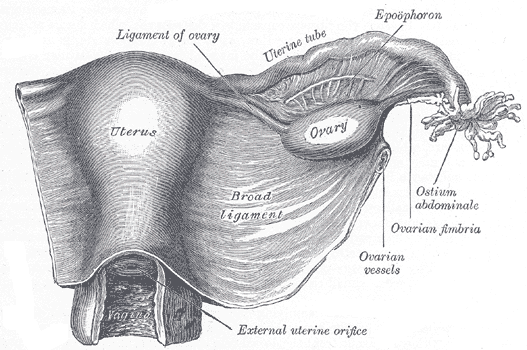
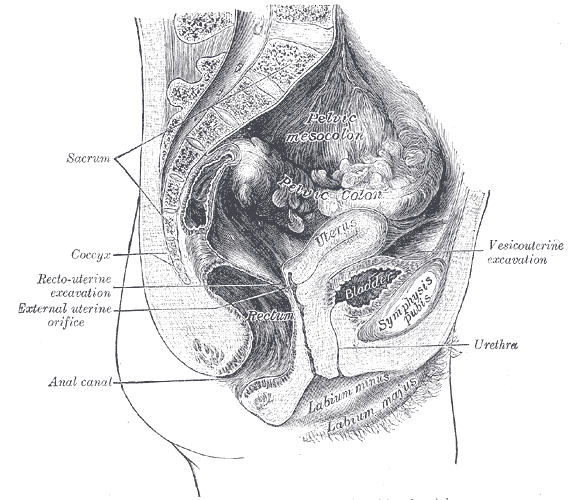
Hysterectomy is simply the removal of the uterus. The tubes and ovaries are not addressed in a hysterectomy.
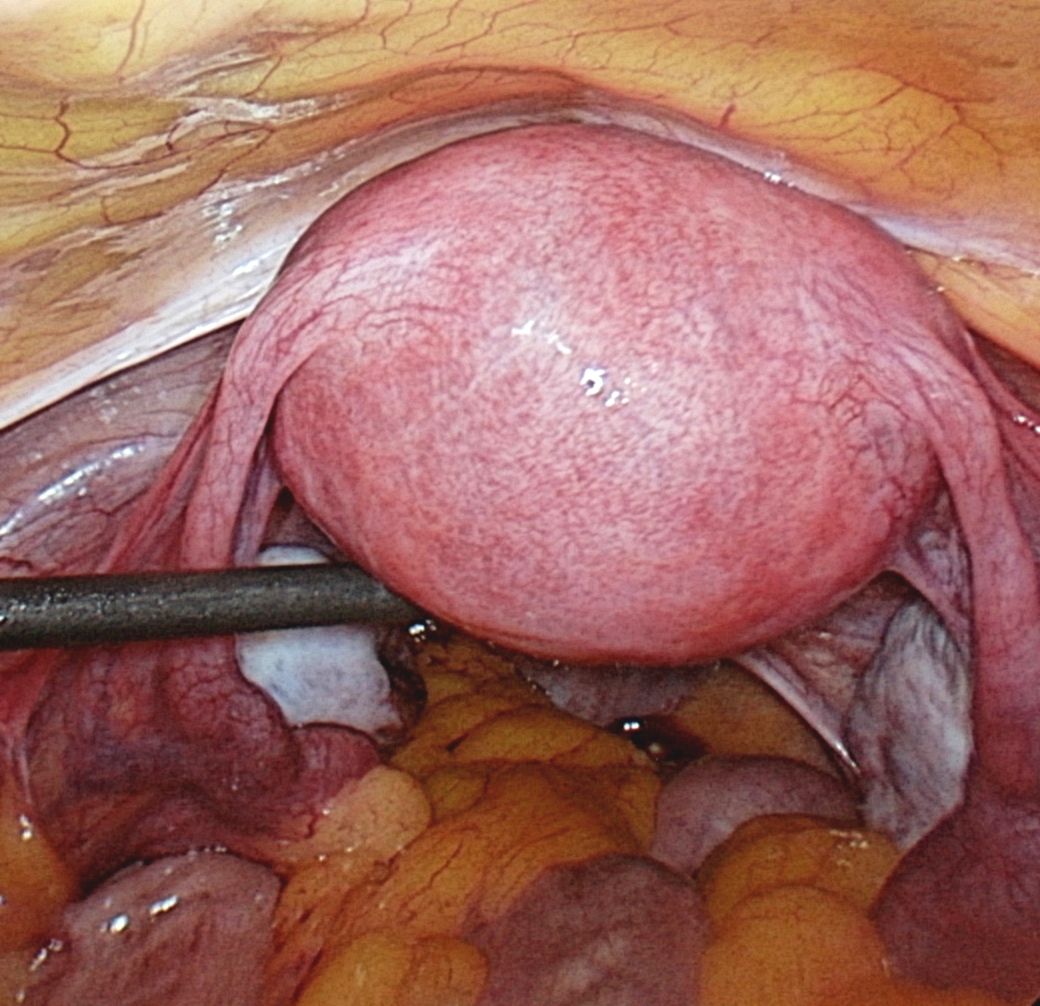
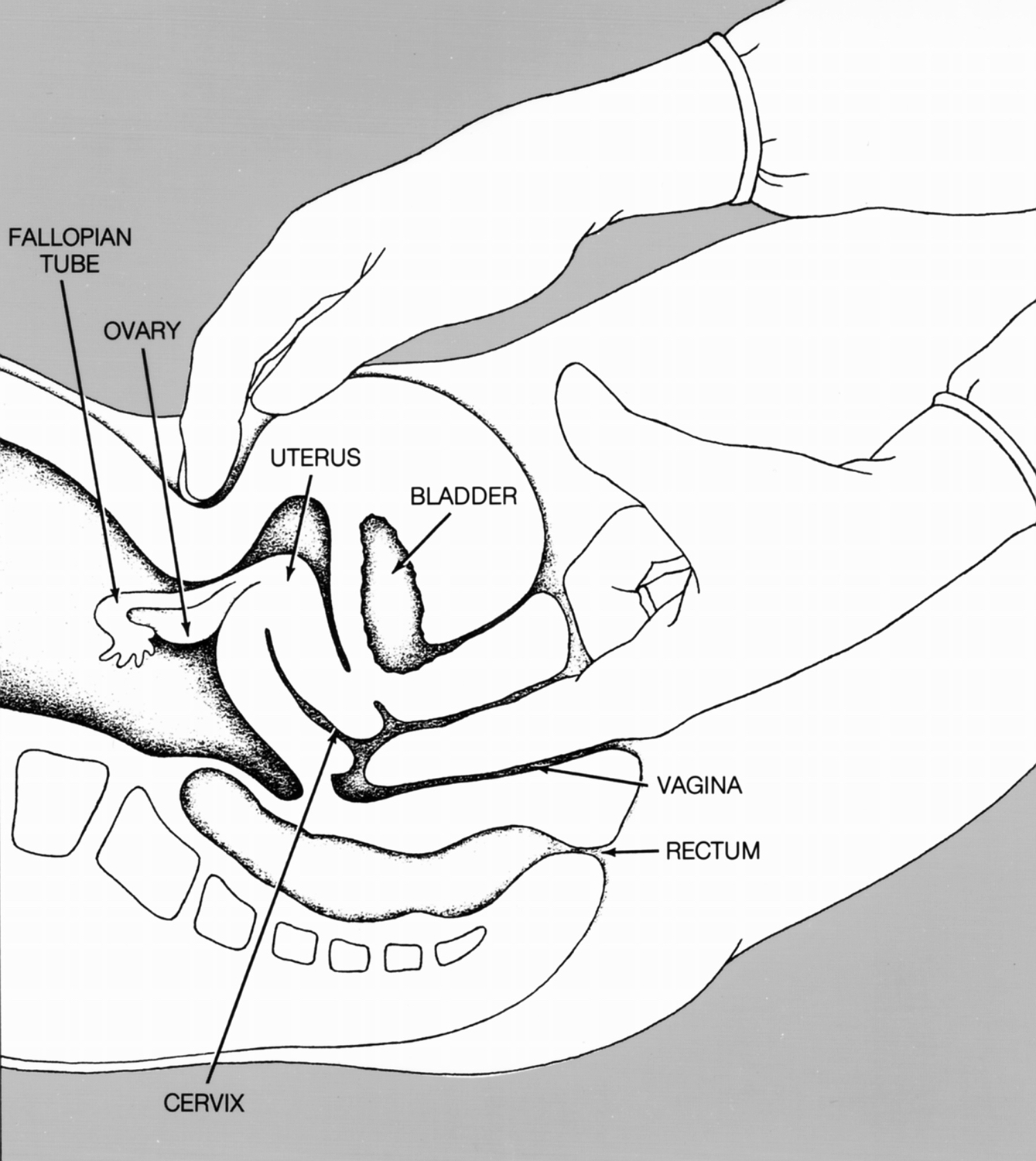
Below you see a series of images designed to give you a feel for the average size, shape and position of the uterus. I myself am highly visual person and feel these will give you a sense of where we are operating when we do a hysterectomy.
Types of hysterectomy
Hysterectomies are done in several ways. Here are the main types:
Thorough the vagina (vaginal hysterectomy)
Through a large incision in the abdomen (open hysterectomy)
Using a laparoscope and simple straight instruments from above for part, and finishing through the vagina for the rest (laparoscopic assisted vaginal hysterectomy- LAVH)
Robotic total abdominal hysterectomy (Using the robot and a laparoscope to do all the work through small ports from above, then when the uterus is totally detached, remove it through the vagina below.)
Please take this time to review the information in the page Laparoscopic and Robotic Surgery.
According to ACOG, about 2/3 of hysterectomies nationwide are still done abdominally. The remaining third are vaginal, laparoscopically assisted or Robotic. The latter third using these methods are considered minimally invasive. It is the goal of ACOG to shift these percentages more toward the minimally invasive techniques. It is also the goal of my practice to utilize such minimally invasive surgical approaches wherever indicated, since they confer many benefits of increased safety and quicker recovery to patients.
Indications for hysterectomy
The only absolute indication for a hysterectomy is uterine cancer. At the same time, there are many other good indications for hysterectomy. Since hysterectomy is a major surgical procedure, we generally prefer considering minor surgical procedures first if applicable, and before those, we prefer medical therapy, if it is appropriate. Nonetheless, many women need and obtain hysterectomies. According to ACOG (The American College of Obstetricians and Gynecologists) :
Hysterectomy is the second most frequently performed major surgical procedure after cesarean delivery among reproductive-age women.
In 2008, the four conditions most often associated with hysterectomy were uterine fibroids, menstrual disorders, uterine prolapse, and endometriosis.
Indications for hysterectomy include:
Fibroids - which cause problems like bleeding or pain, not addressed by other measures
Endometriosis - which causes pain or other problems, not addressed by other methods
Adenomyosis - glandular cells in the muscle wall of the uterus causing swelling and pain
Precancerous or cancerous cells in the uterus
Uterine and other forms of pelvic organ prolapse - not managed by other methods like pessary placement
Please see the sections on Abnormal Uterine Bleeding, Pelvic Pain and Pelvic Relaxation and Prolapse to learn more about the conditions which may be addressed by a hysterectomy.
Risks of hysterectomy
Any surgery, large or small, despite being optimally performed, can have complications. You should be fully familiar with these possibilities before you have any surgery.
For a full accounting of possible complications, please see the section on Consent for Surgery.
When considering the possible complications of a case, don't forget to compare this with possible complications which may occur if you do not have the surgery AND with the possible or probable benefits you stand to gain if you do.
Alternatives to Hysterectomy
To address gynecology problems, we endeavor to obtain a clear diagnosis before prescribing a therapy. Once we determine a clear diagnosis, it is easier to choose a treatment that is likely to work. Most conditions have a least a couple reasonable treatment alternatives. You and your doctor should have a discussion about all the viable alternatives, including their likelihood of being effective for you, their risks, cost, and recovery. You should also discuss whether or not alternative treatments are temporary or partial.
Possible alternative to hysterectomy which may or may not be applicable to any given case are:
D and C, removal of polyps
myomectomy, or removal of fibroids
hormone treatment
endometrial ablation
embolization of vessels in the pelvis
Cautions
Be aware that hysterectomy has become politicized in the media and in our culture. It is important that you steer clear of political or cultural dogma when you are considering your medical treatment options.
When thinking about your health care, learn as much as you can from trusted reputable sources. Consult the internet by all means, but be advised :
Some of the worst quality website content I have seen on the internet has to do with hysterectomy. Ask yourself, do those folks on soapboxes bear any responsibility for your health ? Are they promoting evidence based information ?
See my section on Information and Learning to learn more.
Do not hesitate to get a second opinion about your treatment options. A good doctor will not mind.
Selected FAQS
What is it called when the tubes are removed ? A salpingectomy.
What is it called when the ovaries are removed ? An oophorectomy. To learn more, see Ovarian and Tubal Surgery.
Will a hysterectomy alter my hormones or put me in menopause ? No. Remember a hysterectomy is only removal of the uterus. The ovaries produce the hormones.
Will a hysterectomy alter my sex drive or sexual function ? Generally no. However, if the patient has a hysterectomy for pain or bleeding, it has been my long experience that their post op sexual function improves. It is necessary to wait 6 weeks, sometimes a bit more after a hysterectomy to resume intercourse.
Preparation for Hysterectomy
Check out our page devoted to Surgery FAQs.
Recovery from Hysterectomy
How your recover from hysterectomy depends on your overall health, your outlook, how well you were prepared for your case, your personal support system, whether there were any complications, and how well you follow instructions postoperatively. Patients done using minimally invasive techniques should be back to sedentary jobs by 3-4 weeks post op.
Click here for our actual post op handout.
To learn more:
MedlinePlus, National Institute of Health
PS. Someday if I get around to it, AFTER I get the whole website finished, I will share a bit about my own hysterectomy experience.
Dr. Gina